Respiratory Module 3
Quiz Summary
0 of 34 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 34 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 34
1. Question
A 45-year-old male presents with progressive dyspnea and a non-productive cough over the last six months. His pulmonary function tests (PFTs) reveal a reduced diffusing capacity of the lungs for carbon monoxide (DLCO).
Which of the following best explains the principle underlying the measurement of DLCO in PFTs?
CorrectIncorrect -
Question 2 of 34
2. Question
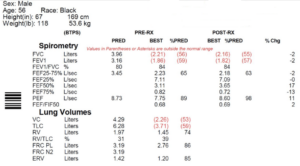
Based on the pulmonary function test (PFT) pattern shown in the attached picture, all of the following conditions could be causes of this patient’s restrictive lung disease except:
CorrectIncorrect -
Question 3 of 34
3. Question
Nintedanib is an intracellular tyrosine kinase inhibitor which has been recently shown to be useful in the treatment of idiopathic pulmonary fibrosis.
Which one is the correct target receptors for this drug?
CorrectIncorrect -
Question 4 of 34
4. Question
Which one of the following paraneoplastic features is least commonly seen in patients with squamous cell lung cancer?
CorrectIncorrect -
Question 5 of 34
5. Question
A 45-year-old patient with a history of HIV/AIDS, currently on antiretroviral therapy but with a recent decline in CD4 count to 180 cells/µL, presents to the emergency department with a 2-week history of progressive dyspnea, non-productive cough, and fever.
The patient was diagnosed with Pneumocystis pneumonia (PCP) based on clinical presentation and a positive sputum PCR for Pneumocystis jirovecii.
Treatment with oral co-trimoxazole was initiated 5 days ago. Despite initial therapy, the patient’s respiratory status has worsened, with increased work of breathing and use of accessory muscles. Arterial blood gas analysis reveals a pO2 of 35 mmHg, indicating significant hypoxia.
Given the patient’s deteriorating condition and hypoxia despite appropriate antimicrobial therapy for PCP, which of the following is the most appropriate treatment to initiate?
CorrectIncorrect -
Question 6 of 34
6. Question
A 40-year-old man with 40 pack year smoking history presents with increasing breathlessness and wheeze. Inspiratory and expiratory flowvolume curves are both “flattened” so that the configuration approaches that of a rectangle.
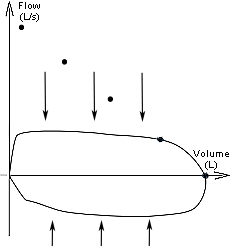
What would be the most likely diagnosis to explain this result?
CorrectIncorrect -
Question 7 of 34
7. Question
A 60-year-old man with 30 pack year smoking history presents with increasing breathlessness and wheeze. A flow volume curve shows that all the flow rates are diminished with mean expiratory flow being less than the mean inspiratory flow rate.
What could be the underlying cause to explain this finding?
CorrectIncorrect -
Question 8 of 34
8. Question
A 43-year-old woman presents with increasing breathlessness and wheeze. Inspiratory and expiratory flow-volume curves show normal inspiration but flow limitation during expiration producing an “expiratory plateau”.
The flow-volume curves are most likely to be caused by:
CorrectIncorrect -
Question 9 of 34
9. Question
A 55-year-old man has the following lung function test results:
- FEV1 2.0 L (61% predicted)
- FVC 2.6 L (68% predicted)
- FEV1/FVC 0.77
- TLC 72% predicted
- RV 75% predicted
- DLCO 64% predicted
- KCO 110% predicted
- His body mass index (BMI) is 31 kg/m2 [18-25].
Which of the following is the best explanation for these results?
CorrectIncorrect -
Question 10 of 34
10. Question
A 50-year-old man has the following lung function test results:
- FEV1 2.0 L (61% predicted)
- FVC 2.6 L (68% predicted)
- FEV1/FVC 77% (80% predicted)
- TLC 70% predicted
- RV 75% predicted
- His body mass index (BMI) is 40 kg/m2 [18-25].
ABG shows normal pH with elevated CO2.
Which of the following is the best explanation for these results?
CorrectIncorrect -
Question 11 of 34
11. Question
A 55-year-old man has the following lung function test results:
- FEV1 2.0 L (61% predicted)
- FVC 2.6 L (68% predicted)
- FEV1/FVC 77% (80% predicted)
- TLC 70% predicted
- RV 75% predicted
- DLCO 48% predicte
His body mass index (BMI) is 31 kg/m2 [18-25]. No bronchodilator response. Normal CXR.
Which of the following is the best explanation for these results?
CorrectIncorrect -
Question 12 of 34
12. Question
A 55-year-old man has the following lung function test results:
- FEV1 1.40 L (56% predicted)
- FVC 1.9 L (57% predicted)
- FEV1/FVC (74% predicted)
- TLC 75% predicted
- RV 75% predicted
- DLCO 35% predicted
- KCO 80% predicted
- 4% improvement in FEV1 after bronchodilator
His body mass index (BMI) is 31 kg/m2 [18-25].
Which of the following is the best explanation for these results?
CorrectIncorrect -
Question 13 of 34
13. Question
Which of the following condition is not associated with increased DLCO?
CorrectIncorrect -
Question 14 of 34
14. Question
You are asked to consult on the aerial transfer of a sick man with bronchopneumonia. By what amount will you expect the alveolar oxygen to drop when the plane is pressurised at an altitude of 5000 feet?
(The atmospheric pressure at 5000 feet is 647 mmHg. The carbon dioxide level is 45 mmHg, the respiratory quotient is 0.8 and the water vapour pressure is 47 mmHg. These values remain constant. The flight will begin at sea level where the atmospheric pressure is 760 mmHg.)CorrectIncorrect -
Question 15 of 34
15. Question
Hypoventilation is the main mechanism for hypoxemia in the following conditions except?
CorrectIncorrect -
Question 16 of 34
16. Question
The alveolar-arterial gradient for oxygen tension in arterial blood (PAaO2) may vary with age.
Which one of the following is considered to be the main physiological mechanism for a normal PA-aO2?
CorrectIncorrect -
Question 17 of 34
17. Question
The mechanism of hypoxemia in interstitial lung disease is mainly due to?
CorrectIncorrect -
Question 18 of 34
18. Question
The PaO2 are shown below for an individual breathing room air and then 100% oxygen: PaO2 (mmHg) 50.0 (breathing air) PaO2 (mmHg) 63.0 (on 100% oxygen)
What would be the best explanation for the above results?
CorrectIncorrect -
Question 19 of 34
19. Question
The following medications causes reduce REM sleep except?
CorrectIncorrect -
Question 20 of 34
20. Question
The following conditions are associated with obstructive sleep apnea except?
CorrectIncorrect -
Question 21 of 34
21. Question
A 43-year-old man is referred for investigation of snoring and witnessed apnoeas. A diagnostic sleep study confirms the diagnosis of obstructive sleep apnea. Therapy with nasal continuous positive airway pressure (CPAP) is recommended.
Which of the following would be the reason why this person would use CPAP for his OSA?
CorrectIncorrect -
Question 22 of 34
22. Question
A 43-year-old male, weighing 100 kg, presents with a 5-year history of excessive daytime sleepiness. He reports a recent motor vehicle accident attributed to falling asleep at the wheel. Subsequent evaluation, including a sleep study, confirms a diagnosis of obstructive sleep apnea (OSA).
What is the most appropriate next step in management?
CorrectIncorrect -
Question 23 of 34
23. Question
Following a polysomnographic evaluation in a patient with a history of left ventricular failure, episodes of decreased oxygen saturation were observed without accompanying respiratory efforts.
What is the most likely explanation for these findings?
CorrectIncorrect -
Question 24 of 34
24. Question
A patient reports experiencing significant discomfort in the legs, primarily at night, described as an irresistible urge to move them.
During a polysomnographic study, frequent, uniform limb movements were recorded, each lasting between 0.5 and 5 seconds, with an amplitude exceeding 25% of toe dorsiflexion measured during calibration.
Laboratory investigations, including a full blood count (FBC) and electrolytes (U&Es), are within normal ranges, yet ferritin levels are found to be low.
What is the most appropriate management approach for this patient?
CorrectIncorrect -
Question 25 of 34
25. Question
A patient presents with excessive daytime sleepiness, cataplexy, sleep paralysis and hypnogogic hallucination.
What is the diagnosis?
CorrectIncorrect -
Question 26 of 34
26. Question
Which of the following medication is least useful in Narcolepsy?
CorrectIncorrect -
Question 27 of 34
27. Question
Which of the following mechanisms is primarily involved in the development of hypertension in patients with obstructive sleep apnea (OSA)?
CorrectIncorrect -
Question 28 of 34
28. Question
A 50-year-old male smoker presents to your clinic complaining of a persistent cough and unexplained weight loss over the past two months.On examination, you note a palpable lymph node in the left supraclavicular fossa.
A chest X-ray (CXR) reveals a “white out” appearance of the left lung, prompting further investigation with a bronchoscopy.
The bronchoscopy results indicate the presence of an undifferentiated carcinoma. Additionally, laboratory tests show elevated levels of serum neuron-specific enolase (NSE).
What is the most likely diagnosis?
CorrectIncorrect -
Question 29 of 34
29. Question
In the management of non-small cell lung cancer, what is the optimal treatment for someone with resectable Stage II disease?
CorrectIncorrect -
Question 30 of 34
30. Question
A 50-year-old male with a significant smoking history presents with a 6-month history of persistent cough and weight loss. More recently, he has experienced progressive weakness in both arms and legs, difficulty with balance and an unsteady gait, and challenges in arising from a seated position and climbing stairs. He also reports symptoms of dry mouth.
Upon physical examination, you observe bilateral ptosis with no significant findings in other cranial nerves. Notably, there is an exaggerated elevation of the eyelids following sustained upward gaze. The patient demonstrates proximal limb weakness, yet without evident muscle wasting, and deep tendon reflexes are absent. Interestingly, muscle strength appears to improve with repeated activity.
Given the neurological findings and the patient’s smoking history, the consulting neurologist raises a suspicion of a paraneoplastic syndrome, likely associated with an underlying malignancy.
What is the most likely underlying malignancy?
CorrectIncorrect -
Question 31 of 34
31. Question
A 32-year-old fit and active male, who is a non-smoker, presents to his general practitioner with a persistent cough and mild dyspnea on exertion. A chest X-ray followed by a CT scan reveals a 3 cm solitary pulmonary nodule in the left upper lobe with no evidence of mediastinal lymph node involvement or distant metastases on PET CT. Biopsy confirms small cell lung cancer (SCLC).
Considering his excellent performance status and limited stage disease, which of the following is the most appropriate initial treatment option?
CorrectIncorrect -
Question 32 of 34
32. Question
Which biomarker has been proposed as a noninvasive diagnostic tool for idiopathic pleuroparenchymal fibroelastosis (PPFE)?
CorrectIncorrect -
Question 33 of 34
33. Question
Which of the following intervention may potentially have a role in idiopathic pleuroparenchymal fibroelastosis (PPFE)?
CorrectIncorrect -
Question 34 of 34
34. Question
A 65-year-old with man with a past medical history of hepatocellular carcinoma was started on nivolumab last month and had underwent 2 cycles. He now presents with worsening shortness of breath and is found to be hypoxic with a resting oxygen saturation of 80 percent on arrival to the emergency department.
His HRCT chest shows diffuse ground glass opacities (GGO’s) and infectious workup including blood cultures, sputum cultures and pneumonia workup were all found to be unremarkable.
The following interventions would all be appropriate except?
CorrectIncorrect
