Copy of Respiratory Module 1
Quiz Summary
0 of 38 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 38 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 38
1. Question
A 65-year-old man presents with symptoms of paroxysmal nocturnal dyspnea on a background of known ischaemic heart disease. He had an echocardiogram performed last month which revealed a left ventricular ejection fraction of 25%. The respiratory parameters from a polysomnographic sleep study are shown below:
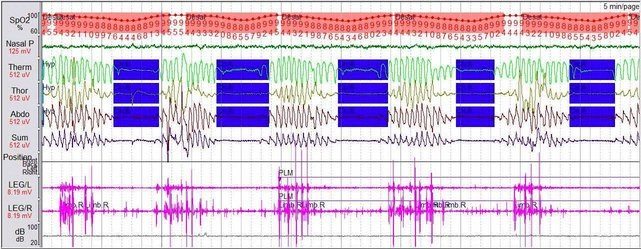
What is the most likely explanation for the change?
CorrectIncorrect -
Question 2 of 38
2. Question
In patients with moderate to severe obstructive sleep apnea, treatment with CPAP is unlikely to achieve the following outcome:
CorrectIncorrect -
Question 3 of 38
3. Question
A 45 year old man is diagnosed with obstructive sleep apnea. His AHI is 50 events/ hour on an overnight sleep study. He has had a trial of CPAP at home which reduced his AHI to less than 5 events/hr, but found CPAP intolerable. Since he stopped using it, his daytime somnolence had become worse.
What other alternative does he have?
CorrectIncorrect -
Question 4 of 38
4. Question
A 67 year old man with a BMI of 40 has been diagnosed with bulbar motor neuron disease for the last two years. He sees you in clinic complaining of having excess daytime sleepiness and had an Epsworth sleepiness score of 16/24.
He then proceed to have a level III sleep study (Embletta system) which revealed the following information:
- Overall AHI 39.9
- Oxygen saturation average 95.1%
- Frequent Hypopnoea and Obstructive Apnoea occurred during the sleep period with an average duration of 19.2 seconds
- Average Oxygen desaturation to below 90% in 5.3% of the recording time.
His spirometry shows an FEV1 of 2.82 (78% predicted), FVC 3.81 (74% predicted), Ratio 0.78.
Apart from commencing a trial of CPAP, which of the following is the most appropriate next step in management?
CorrectIncorrect -
Question 5 of 38
5. Question
A patient with a mutation in the PHOX2B gene will most likely benefit from the following intervention:
CorrectIncorrect -
Question 6 of 38
6. Question
During diving, there is a change in external pressure as the depth of the dive changes.
According to Boyle’s Law, what actually occurs as a free diver rises to the surface?
CorrectIncorrect -
Question 7 of 38
7. Question
Selexipag is a selective prostacyclin-receptor agonist with a recognized role in the treatment of pulmonary arterial hypertension.
What is the most common side effect associated with this medication?
CorrectIncorrect -
Question 8 of 38
8. Question
Riociguat is a member of a new class of therapeutic agents called soluble guanylate cyclase stimulators and is useful in which of the following condition?
CorrectIncorrect -
Question 9 of 38
9. Question
A 60 year old man undergoes a right heart catheter study and his results are as follows:
- mPAP 23 mmHg
- PAWP 10 mmHg
- PVR 3 WU
Based on the above haemodynamic profile, where is the most likely anatomical location for this man’s pulmonary hypertension?
CorrectIncorrect -
Question 10 of 38
10. Question
In the treatment of pulmonary hypertension, vasodilator therapy should be avoided in which of the following patient group?
CorrectIncorrect -
Question 11 of 38
11. Question
Inhaled Treprostinil have shown promising results in the treatment of which group of pulmonary hypertension?
CorrectIncorrect -
Question 12 of 38
12. Question
If an average 70kg man has a respiratory rate of about 18 breaths per minute and a tidal volume of 600 mL. What would his pulmonary ventilation be?
CorrectIncorrect -
Question 13 of 38
13. Question
A 40 year old man complains of increasing dyspnea, worsening cough with increased sputum production and recurrent lower respiratory tract infection. He is infertile and has had a previous sinus surgery for recurrent nasal polyps and recurrent sinusitis. He has signs of situs inversus on examination.
Which of the following would provide the least useful information in establishing a diagnosis for this man?
CorrectIncorrect -
Question 14 of 38
14. Question
Which of the following intervention has NOT been proven to improve survival in patients with chronic obstructive pulmonary disease (COPD)?
CorrectIncorrect -
Question 15 of 38
15. Question
You are seeing a 65 year old man with severe COPD in clinic . His FEV1 is 28% predicted. However his disease has been stable on 3 bronchodilators (tiotropium,salmeterol and fluticasone) and had only one admission in the last four years following an infective exacerbation of his COPD. Given the stability of his condition, you decide to slowly withdraw his inhaled dose of fluticasone over a 3 month period.
What could potentially happen to him in the next 12 months following the withdrawal of his inhaled corticosteroid?
CorrectIncorrect -
Question 16 of 38
16. Question
A 70-year-old man with a history of severe chronic obstructive pulmonary disease (COPD) presents to your clinic for a routine review. He has been diagnosed with an FEV1 of 30% indicating severe obstruction. His symptom burden is high with a COPD Assessment Test (CAT) score of 20, and he experiences significant dyspnea as reflected by a Modified Medical Research Council (MMRC) dyspnea scale score of 3.
Over the past year, he has been hospitalized twice due to infective exacerbations of his COPD.
His current medication regimen includes Salmeterol/Fluticasone inhaled twice daily and Salbutamol as needed for acute symptom relief. Considering his frequent exacerbations and current symptom burden, you consider optimizing his inhaler therapy.
Which of the following inhaler changes would be most beneficial in preventing future COPD exacerbations for this man?
CorrectIncorrect -
Question 17 of 38
17. Question
The use of high flow nasal oxygen is increasingly recognized as an important treatment modality for patients with acute hypoxemic respiratory failure.
The following are benefits of such therapy compared to non-invasive ventilation, except?
CorrectIncorrect -
Question 18 of 38
18. Question
Which of the following statement regarding Preserved Ratio Impaired Spirometry (PRISm) is incorrect?
CorrectIncorrect -
Question 19 of 38
19. Question
A 56 year old man with a background of moderate COPD (FEV1 60% predicted) presents to your clinic for a review. He is an ex-smoker of 30 pack years. On your clinical assessment, he has a CAT score of 12 and mMRC of 2. His resting oxygen saturation is 90 percent on air. Over the last 12 months, he has presented twice to the emergency department with COPD exacerbations requiring antibiotic and steroid therapy. He is currently taking umeclidinium bromide 62.5mcg inhaled once daily and uses Salbutamol as required.
All of the following treatment advice would be appropriate for this man except?
CorrectIncorrect -
Question 20 of 38
20. Question
The upper respiratory tract consists of the nasal cavity, pharynx and larynx. The lower respiratory tract consists of the trachea, bronchi and lungs.
If a person accidentally inhales a foreign object, for example a peanut, where in the respiratory tract is it most likely to lodge?
CorrectIncorrect -
Question 21 of 38
21. Question
Which of the following patient group would most likely benefit from endobronchial valve placement?
CorrectIncorrect -
Question 22 of 38
22. Question
A D-dimer with a threshold of 500 mcg/L has been shown to be a highly sensitive test with a correspondingly high negative predictive value among patients with low pretest probability for PE. However, the Ddimer level tends to increase with age.
If so, what would be an optimal D-dimer cutoff value for a 63 year old?
CorrectIncorrect -
Question 23 of 38
23. Question
Rivaroxaban is a direct oral anti-coagulant that is indicated for the treatment of DVT and PE.
Which of the following scenario could potentially determine its preference over oral Dabigatran?
CorrectIncorrect -
Question 24 of 38
24. Question
A 52-year-old previously healthy man from Queensland presents to the emergency department with acute onset of dyspnea. He is visibly in severe respiratory distress, with a respiratory rate of 40 breaths per minute, a pulse rate of 120 beats per minute, and blood pressure measuring 100/60 mmHg. His oxygen saturation is 85% on room air.
A bedside echocardiogram reveals signs of right ventricular strain, suggestive of acute pulmonary hypertension.
The initial ECG demonstrates an incomplete right bundle branch block. Laboratory investigations reveal a troponin level of 120 ng/L and a pro-BNP level of 1500 pg/mL, indicating cardiac strain.
An urgent CT Pulmonary Angiography (CTPA) is performed, confirming a large saddle embolus obstructing the right main pulmonary artery, a critical finding that necessitates immediate intervention.
Given the severity of the presentation and the imaging findings, systemic thrombolysis would typically be considered. However, due to specific patient factors or potential contraindications to systemic thrombolysis, the decision is made to proceed with catheter-directed thrombolysis (CDT) in the catheterization laboratory.
What is the major advantage of catheter-directed thrombolysis (CDT) over systemic thrombolysis in the management of a large pulmonary embolism as described in this patient?
CorrectIncorrect -
Question 25 of 38
25. Question
A 70 year old man with a background of severe COPD with an FEV1 of 20% is being discharged from the ward today following a week long admission with severe infective exacerbation of COPD requiring a period of non-invasive ventilation.
Which of the following index will best predict his hospital readmission in the next 3 months?
CorrectIncorrect -
Question 26 of 38
26. Question
A 70 year old woman with known COPD is admitted to hospital with a two day history of worsening reathlessness, cough and sputum production. Clinically she is tachypneic with a RR of 40 and saturating 89% on 2L/min of oxygen. Her arterial blood gas shows acute respiratory acidosis with a pH of 7.20 and a pCO2 of 100.
Which of the following intervention will most likely reduce her risk of needing invasive intubation and ventilation?
CorrectIncorrect -
Question 27 of 38
27. Question
In the management of community acquired pneumonia, which of the following clinical tool has the highest accuracy of predicting patients who will require intensive respiratory and ventilatory support (IRVS)?
CorrectIncorrect -
Question 28 of 38
28. Question
What is the antibiotic of choice for severe community acquired pneumonia in patients living in a non-tropical region in Australia?
CorrectIncorrect -
Question 29 of 38
29. Question
Which of the following primary lung cancer has the most favourable prognosis?
CorrectIncorrect -
Question 30 of 38
30. Question
Glycopyrronium bromide is an inhaled long-acting muscarinic antagonist (LAMA) that is used as a maintenance bronchodilator treatment to relieve symptoms in adults with chronic obstructive pulmonary disease (COPD).
What is the most common side effect of this medication?
CorrectIncorrect -
Question 31 of 38
31. Question
With regards to Positron Emission Tomography (PET) scanning, which of the following statement below is incorrect?
CorrectIncorrect -
Question 32 of 38
32. Question
In individuals with persistent symptoms of asthma, treatment with an inhaled corticosteroid will improve the following except?
CorrectIncorrect -
Question 33 of 38
33. Question
Which of the following malignancies has the highest mortality rate in Australia?
CorrectIncorrect -
Question 34 of 38
34. Question
A 35-year-old man presents with fever, malaise, a red indurated rash on his lower leg and marked painful swelling of both ankles. His chest X-ray is shown below:
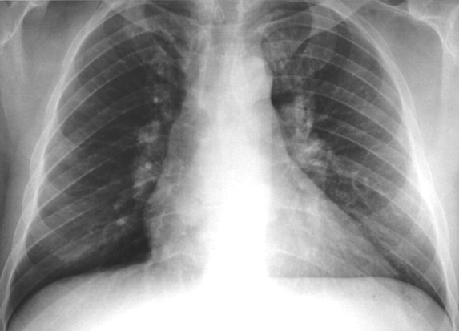
What is the most likely diagnosis?
CorrectIncorrect -
Question 35 of 38
35. Question
A 37 year old man from Wellington, previously fit and well, presents with two months history of general unwellness with increased lethargy, abdominal pain and headache. He is a current smoker of 10 pack years. Examination is unremarkable. His serum sodium, potassium and creatinine are all within normal limits.
However he does have a raised serum corrected calcium of 3.5mmol/L and a suppressed serum PTH of 0.6 pmol/L. His chest X-ray shows prominent bilateral hilar lymphadenopathy.
What is the most likely explanation for his hypercalcemia?
CorrectIncorrect -
Question 36 of 38
36. Question
A 66-year-old man with a 50-pack-year smoking history presents for assessment of disabling dyspnoea and reduced exercise tolerance. Physical examination reveals poor chest expansion with increased percussion note and vesicular but globally reduced breath sounds. There is no evidence of cardiac failure.
His pulmonary function tests show a forced expiratory volume in 1 second (FEV1) of 0.89 L (predicted 2.95 L) and a forced vital capacity (FVC) of 2.10 L (predicted 3.65 L). After bronchodilator, FEV1 increased to 1.1 L and FVC to 3.0 L. Residual volume was 185% predicted, carbon monoxide diffusing capacity was 50% predicted and his resting SaO2 was 95% on room air.
You decide to refer him to the pulmonary rehabilitation program.
Which one of the following is least likely to improve after completion of a pulmonary rehabilitation program?
CorrectIncorrect -
Question 37 of 38
37. Question
The following are potential biomarkers for a guarded prognosis from COVID-19 pneumonia except?
CorrectIncorrect -
Question 38 of 38
38. Question
The following vaccines are recommended for all patients with stable COPD except?
CorrectIncorrect
