Gastroenterology Module 4
Quiz Summary
0 of 29 Questions completed
Questions:
Information
You have already completed the quiz before. Hence you can not start it again.
Quiz is loading…
You must sign in or sign up to start the quiz.
You must first complete the following:
Results
Results
0 of 29 Questions answered correctly
Your time:
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0)
0 Essay(s) Pending (Possible Point(s): 0)
| Average score |
|
| Your score |
|
Categories
- Not categorized 0%
- 1
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- Current
- Review
- Answered
- Correct
- Incorrect
-
Question 1 of 29
1. Question
The manometric feature most characteristic of achalasia is:
CorrectIncorrect -
Question 2 of 29
2. Question
A 16 year old male presents with recurrent episodes of obstructive dysphagia. Over the past year he has required endoscopic removal of impacted food in the upper oesophagus on several occasions. A barium meal is normal.
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 3 of 29
3. Question
A 21 year old man presents with dysphagia and regurgitation of undigested food. His barium swallow images are shown below.
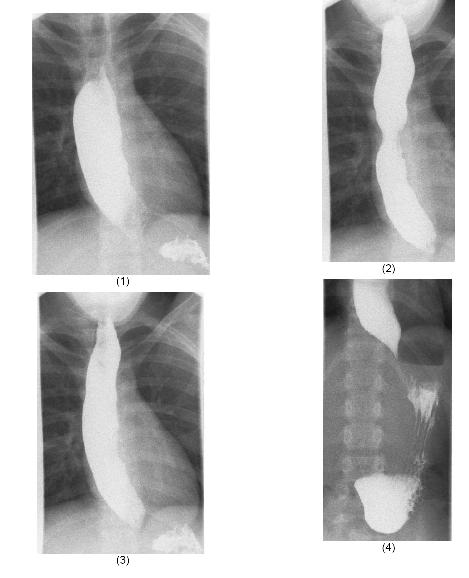
What is the most likely diagnosis?
CorrectIncorrect -
Question 4 of 29
4. Question
An obese male patient presents with 3 months history of reflux symptom.Endoscopy done 2 weeks ago was normal. He undergoes an ambulatory pH monitoring.
The result as follow:
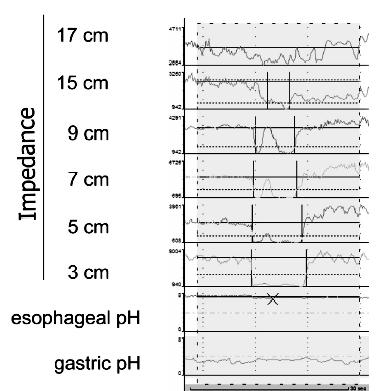
What is the most likely diagnosis?
CorrectIncorrect -
Question 5 of 29
5. Question
Which of the following organism is a known cause of secondary achalasia?
CorrectIncorrect -
Question 6 of 29
6. Question
A 68-year-old man is sent for a second opinion regarding recurrent iron deficiency anaemia requiring blood transfusion.
Over the last three years, he has required an average of 4 units of packed cells every three months despite oral iron supplements. There is no history of melaena. Bone marrow examination is normal except for absent iron stores.
Gastroscopy and colonoscopy have been negative on three separate occasions, the last being two months ago. Small bowel biopsy is normal. The patient had a barium meal and follow-through six months ago which was normal.
General health is good and he is on no regular medications.
Which of the following investigations is most likely to find the cause of his iron deficiency?
CorrectIncorrect -
Question 7 of 29
7. Question
A 45-year-old woman is evaluated for a 2-week history of right leg and flank pain and a slight limp. The patient was diagnosed with Crohn disease at age 20 years when she was evaluated for abdominal pain, nausea, and vomiting, and small-bowel radiographic series revealed a stenotic area in her terminal ileum with proximal dilatation and an enteroenteric fistula.
She had an elective ileocolic resection with a primary anastomosis when her disease proved to be refractory to corticosteroid therapy. She has since been pain-free but has required intermittent courses of antibiotics and mesalamine for diarrheal flares of disease. She has had routine colonoscopic examinations with colonic biopsies showing scattered aphthous ulcerations and biopsy specimens revealing non-necrotizing granulomas in the colon and neo-terminal ileum.
Her most recent colonoscopy was 5 years ago. She is otherwise healthy and takes no medication.
On physical examination, the temperature is 38.0 °C, the blood pressure is 120/80 mm Hg, and the pulse rate 90/min; there is right-sided abdominal tenderness and restricted painful extension of the right hip; otherwise, the range of motion of the hip is normal and without pain. She has an abnormal gait, favoring her right leg.
Which of the following is the most likely diagnosis?
CorrectIncorrect -
Question 8 of 29
8. Question
A 57-year-old woman is evaluated for a 1-month history of increased abdominal girth. The patient has a 15-year history of alcohol abuse, drinking a bottle of wine a day. She also has type 2 diabetes mellitus, hypertension, and hyperlipidemia, and her medications are metformin, hydrochlorothiazide, propranolol, simvastatin, and aspirin.
On physical examination, the temperature is 37.1 °C , the blood pressure is 90/50 mm Hg, the pulse rate is 99/min, and the respiration rate is 13/min; the BMI is 21. Examination reveals scleral icterus; bulging flanks; small umbilical hernia; caput medusae; spider angiomata of the face, arms, and chest; and mild asterixis. There is no abdominal tenderness.
Laboratory studies:
- Leukocyte count 5200/µL (5.2 × 109/L) with a normal differential
- Platelet count 65,000/µL (65 × 109/L)
- INR 2.2
- Bilirubin (total) 3.4 mg/dL (58.1 µmol/L)
- Bilirubin (direct) 1.8 mg/dL (30.8 µmol/L)
- Aspartate aminotransferase 120 U/L
- Alanine aminotransferase 65 U/L
- Alkaline phosphatase 196 U/L
- Albumin 2.7 g/dL (27 g/L)
- Creatinine 2.7 mg/dL (206.0 µmol/L)
- Urinalysis Normal
- Blood cultures are negative.
Ultrasonography of the abdomen shows massive ascites, patent vessels, no ductal dilatation, and a shrunken liver with no masses.
Which of the following is the most appropriate management for this patient?
CorrectIncorrect -
Question 9 of 29
9. Question
The most common cause for asymptomatic, mildly elevated serum transaminases in Western society is:
CorrectIncorrect -
Question 10 of 29
10. Question
Which of the following intervention has the most robust evidence of causing sustained improvement in liver histology in obese patients with non-alcoholic steato-hepatitis (NASH)?
CorrectIncorrect -
Question 11 of 29
11. Question
A 53-year-old man is evaluated after a recent episode of substernal chest pain. He was evaluated in the emergency department for chest pain, and serial electrocardiograms and measurement of cardiac enzymes showed no evidence of myocardial ischemia. An outpatientstress test also showed no evidence of myocardial disease. The patient has a history of medically controlled hypertension, and his only medication is amlodipine.
On physical examination, the patient appears healthy and vital signs are normal. Barium esophagography shows a segmented or corkscrew esophagus. Esophageal manometry shows simultaneous contractions in the distal esophagus with 50% of swallows.
Which of the following is the most appropriate therapy for this patient?
CorrectIncorrect -
Question 12 of 29
12. Question
A patient who has undergone bariatric surgery now presents with diarrhea, bloating and weight loss.
- Upper and lower GI scope normal
- Tissue transglutaminase Ab negative
- Stool culture for ova cyst and parasite negative
What is the most likely diagnosis?
CorrectIncorrect -
Question 13 of 29
13. Question
What is the most common precipitant of esophageal squamous cell carcinoma?
CorrectIncorrect -
Question 14 of 29
14. Question
A 78 year old man develops sudden onset of projectile vomiting followed by watery diarrhea which started within 24 hours following his return from a Cruise ship in Auckland.
Which is the culprit organism responsible for his current illness?
CorrectIncorrect -
Question 15 of 29
15. Question
In the management of hepatic encephalopathy, what is the main therapeutic effect of lactulose?
CorrectIncorrect -
Question 16 of 29
16. Question
In patients with Crohn’s, this genetic variant would lead to early initial surgery due to stricturing disease:
CorrectIncorrect -
Question 17 of 29
17. Question
In patients with colitis, the cumulative cancer risk is highest after how many years of having the disease?
CorrectIncorrect -
Question 18 of 29
18. Question
Which of the following cytokine is not involved in the pathogenesis of Crohn’s disease?
CorrectIncorrect -
Question 19 of 29
19. Question
The following are predictors of severity in Crohn’s disease except?
CorrectIncorrect -
Question 20 of 29
20. Question
A patient is suspected to have colitis. Blood test shows pANCA positive and ASCA negative.
What might be the suggested diagnosis here?
CorrectIncorrect -
Question 21 of 29
21. Question
A patient with ulcerative colitis has been treated with sulfasalazine for 3 months without achieving disease control.
What is the most appropriate next step in management?
CorrectIncorrect -
Question 22 of 29
22. Question
The initial luminal digestion of dietary starch by salivary and pancreatic amylase leads to the formation of which disaccharide?
CorrectIncorrect -
Question 23 of 29
23. Question
What is the mode of action of infliximab?
CorrectIncorrect -
Question 24 of 29
24. Question
Which of the following is the most common gene mutation seen in HNPCC?
CorrectIncorrect -
Question 25 of 29
25. Question
Which one of the following is least associated with hepatocellular carcinoma?
CorrectIncorrect -
Question 26 of 29
26. Question
A 44-year-old man develops stage C cancer of the caecum. There is no history of colitis but there is a strong family history of bowel cancer in the absence of polyps.
The most likely underlying inherited genetic abnormality is in:
CorrectIncorrect -
Question 27 of 29
27. Question
A 35-year-old man presents with rectal bleeding. He describes the blood as being mixed with the stool. He is otherwise well. His brother was diagnosed with bowel cancer at the age of 38.
At colonoscopy he was found to have two exophytic tumours, one at the hepatic flexure, the other in the distal transverse colon. The remainder of the colon was normal. Biopsies of both areas showed adenocarcinoma.
The most likely genetic disorder in this family is:
CorrectIncorrect -
Question 28 of 29
28. Question
This extra-colonic malignancy is most strongly associated with HNPCC
CorrectIncorrect -
Question 29 of 29
29. Question
This particular patient feature is most suggestive of hereditary nonpolyposis colon cancer (HNPCC):
CorrectIncorrect
